一、Pulmonary arterial hypertension
Pulmonary arterial hypertension (PAH) is refers to a clinical and pathophysiological syndrome characterized by changes in pulmonary vascular structure or function due to various heterogeneous diseases (etiologies), different pathogeneses, and different onset mechanisms, leading to an increase in pulmonary vascular resistance and pulmonary arterial pressure. This syndrome can progress to right heart failure and even death. PAH is a serious, irreversible, progressive, and fatal health condition[1]. There is limited epidemiological data on PH worldwide. In the UK, PH has a prevalence of 97 cases per million, with a female-to-male ratio of 1.8:1. The epidemiology of different PAH types varies, with internationally registered studies reporting an incidence of approximately 2.4 per million person-years and a prevalence of about 15 per million. Common causes of PAH include congenital heart disease, hereditary factors, and exposure to certain drugs or toxins, while connective tissue disease (CTD) is the most prevalent contributing factor[4].
Pulmonary arterial hypertension patients face challenges in early diagnosis, treatment, and have a grim prognosis. Often, they succumb to unmanageable right heart failure once symptoms manifest.

二、Clinical classification of pulmonary arterial hypertension
In clinical terms, PH is categorized into five groups: (1) Pulmonary arterial hypertension (PAH); (2) PH due to left heart disease; (3) PH linked to pulmonary diseases and/or hypoxia; (4) PH due to chronic thromboembolic pulmonary hypertension (CTEPH) and/or PH due to other pulmonary artery blockages; and (5) PH of unknown origin and/or arising from multiple factors.
三、Clinical manifestations
Clinical symptoms of pulmonary hypertension (PH) lack specificity and primarily manifest as progressive right heart dysfunction-related symptoms, often triggered by exertion. These symptoms often include fatigue, dyspnea, chest tightness, chest pain, and syncope. Some patients may also experience a dry cough and exercise-induced nausea and vomiting. In later stages, patients may suffer symptomatic attacks even at rest, leading to swelling in the ankles, lower limbs, and potentially the abdomen and entire body as right heart dysfunction worsens. Underlying or associated conditions that lead to PH may exhibit their own clinical features. Additionally, some patients may experience complications of PH and abnormal pulmonary blood flow distribution, resulting in symptoms such as hemoptysis, hoarseness, and chest pain. Severe dilation of the pulmonary artery can even give rise to pulmonary artery rupture or dissection.
四、Clinical severity assessment
Pulmonary arterial hypertension (PAH) clinical severity assessment involves a comprehensive evaluation of the patient's condition and prognosis, utilising various examination indicators like clinical symptoms, WHO functional classification, 6-minute walk test (6MWT), cardiopulmonary exercise testing, echocardiography, cardiac magnetic resonance (CMR), hemodynamics, and serum biomarkers. This assessment significantly aids in guiding treatment and evaluating efficacy.
五、PAH treatment
In recent years, substantial breakthroughs have been made in pharmacological and therapeutic approaches for various etiologies of Pulmonary Arterial Hypertension (PAH). Nonetheless, a substantial number of patients continue to suffer from disease progression despite optimal drug therapy, leading to a decline in their quality of life, increased readmission rates, and escalating medical expenses. Idiopathic Pulmonary Arterial Hypertension (IPAH) carries an annual mortality of approximately 10%, and regrettably, it remains incurable. In specific conditions such as scleroderma-associated PAH, the mortality is even higher
For patients with drug-resistant and high-risk PAH, the only recourse is often urgent double lung transplantation. However, this option is available to only a small fraction of PAH patients, as merely 3% of those with pulmonary arterial hypertension are suitable candidates for lung transplantation. While the median post-transplant survival stands at 6.7 years, PAH still exhibits a higher mortality rate compared to other medical conditions.
Current pulmonary arterial hypertension (PAH) treatment alternatives encompass general approaches, basic therapies, specific therapies, balloon atrial septostomy (BAS), and lung transplantation. Basic treatment involves the administration of anticoagulants, diuretics, and oxygen therapy. Specific therapy entails targeted drugs such as endothelin receptor antagonists, phosphodiesterase type 5 (PDE5) inhibitors, and soluble guanylate cyclase agonists.
BAS, a procedure that creates a controlled right-to-left shunt through an atrial septal balloon, can reduce right heart pressure and alleviate right heart failure. However, there's a crucial concern: an excessively large shunt may induce severe hypoxia, elevating the patient's mortality risk. Conversely, a too-small shunt can result in rapid spontaneous healing in 25% of patients with atrial septum stomas, necessitating repeated BAS procedures.
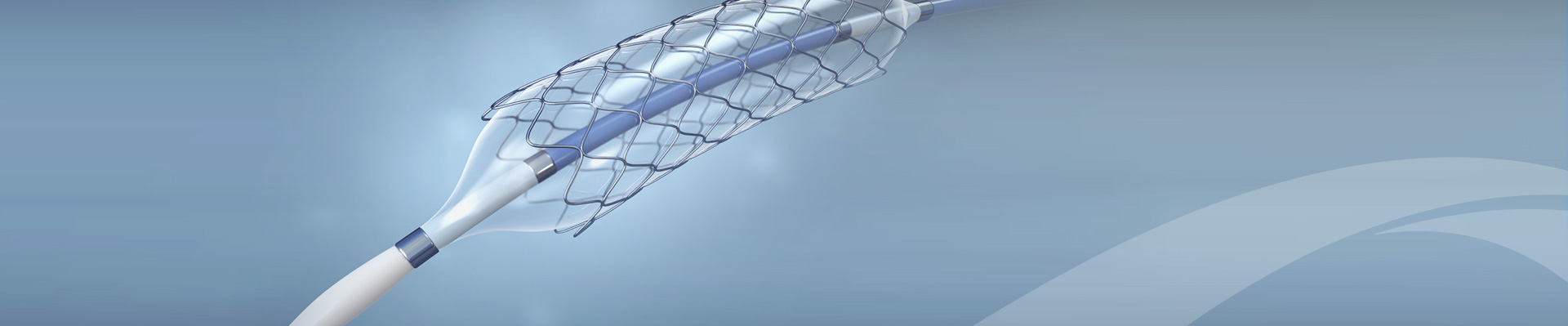
Thus, precise flow rate control to limit the right-to-left shunt is of paramount importance. A dedicated atrial septal shunt has been specifically designed and developed to serve this purpose, representing a promising advancement in PAH treatment instruments in recent years.
六、Atrial septum shunt device
Atrial septal shunt devices symbolize a promising global advancement in treating PAH. In comparison to traditional approaches, they offer broad applicability, cost-effectiveness, and ease of adoption. These devices effectively lower right atrial pressure, easing pulmonary congestion and breathing issues by constricting the atrial septum's diameter. On top of that, they do not significantly burden the right heart or reduce cardiac output, nor do they pose a risk of abnormal embolism.
Currently, three foreign atrial septal shunt devices (Corvia IASD, Israel V-Wave, Occlutech AFR) have obtained CE certification, while there are no equivalent products available in China, where all are still in the clinical research stage. As clinical research results continue to emerge, this technology holds the potential to revolutionize heart failure treatment in Mainland China, offering an economical, safe, and effective alternative for PAH patients [5].
References:
[1] Xiao Shuna et al., Application of atrial septal shunt in patients with severe pulmonary hypertension. Chinese Clinical Journal of Thoracic and Cardiovascular Surgery, 2022. 29(11): pp. 1525-1531.
[2]Humbert, M., et al., Pulmonary Arterial Hypertension in France: Results from a National Registry. American Journal of Respiratory and Critical Care Medicine, 2006. 173(9): p. 1023-1030.
[3].McGoon, M.D., et al., Pulmonary Arterial Hypertension Epidemiology and Registries. Journal of the American College of Cardiology, 2013. 62(25): p. D51-D59.
[4].Pulmonary Embolism and Pulmonary Vascular Disease Group, Respiratory Disease Branch of Chinese Medical Association, Respiratory Physician Branch of Chinese Medical Doctor Association, National Pulmonary Embolism and Pulmonary Vascular Disease Prevention and Treatment Collaboration Group, National Pulmonary Hypertension and Standardization System Construction Project Expert Group, Chinese Guidelines for the Diagnosis and Treatment of Pulmonary Arterial Hypertension (2021 Edition). Chinese Medical Journal, 2021. 101(01): pp. 11-51.
[5]Tian Jun et al., Clinical research progress of atrial septal shunt device. Chinese Journal of Cardiovascular Research, 2021. 19(01): pp. 86-89.
Pursue further excellence!